Research results say: COVID-19 leads to vascular inflammation, heart attack, stroke
Currently multiple research results describe COVID-19 as less of a lung disease and more of a systemic vascular disease that may lead to strokes. Accordingly, the coronavirus affects not only the respiratory tract, but also the neurovascular unit, which supplies vital organs – the brain, kidneys and lungs.
SARS-CoV-2 infection can be particularly dangerous in patients whose vascular function is already impaired by pre-existing conditions. This explains the typical clinical picture by causing circulatory disorders in the heart, as well as pulmonary embolism and vascular occlusions in the brain and kidneys. These can eventually lead to fatal multi-organ failure. The scientists emphasize that it is mainly multi morbid patients with cardiovascular risk factors such as high blood pressure, high blood lipids (hypercholesterolaemia), high blood sugar levels (Diabetes mellitus) and patent foramen ovale (PFO) who are seriously affected by COVID-19.
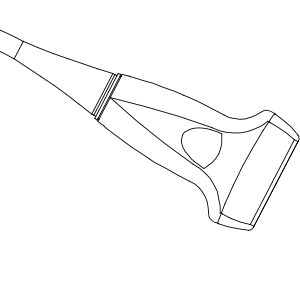
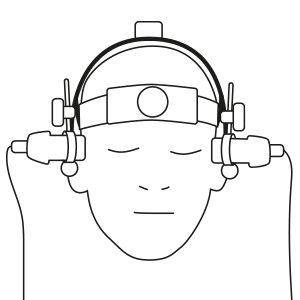
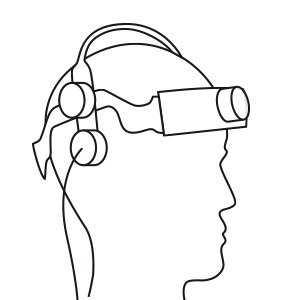
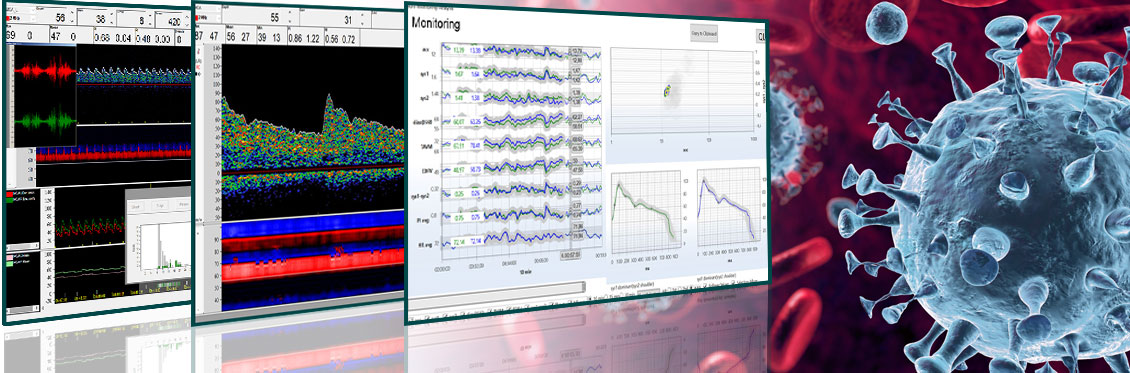
TCD for early detection and therapy determination
With the help of TCD screening, the risk of vascular diseases can be diagnosed in COVID-19 patients and a targeted decision about their therapy and treatment can be made.
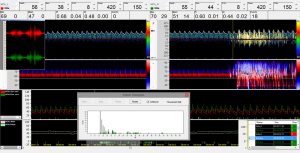
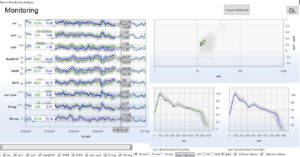
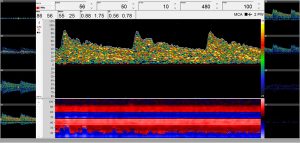
If the coronavirus causes vascular inflammation (vasculitis), the inflammatory reaction leads to vascular narrowing with relevant relevant cerebral blood flow velocities (CBFV) changes. An intracranial routine examination can assist in diagnosis of vasculitis by following proximal cerebral vascular abnormalities.
Emboli detection and a TCD-based PFO test can indicate an increased risk of thrombosis and stroke in COVID-19 patients. Therefore, a therapy can be determined more precisely and the patient can be protected against possible consequential damage with appropriate measures.
Since inflammation of the vascular system has a serious influence on the blood flow velocities, the course of the disease and therapy of a patient affected by COVID-19 can be controlled and optimized using the Neuromonitoring Analysis (NMA).
Literature
Vascular Events in COVID-19
The Spectrum of Neurologic Disease in the Severe Acute Respiratory Syndrome Coronavirus 2 Pandemic Infection – Neurologists Move to the Frontlines; Samuel J. Pleasure, MD, PhD; Ari J. Green, MD; S. Andrew Josephson; JAMA Neurol. Published online April 10, 2020. DOI: 10.1001/jamaneurol.2020.1065 https://jamanetwork.com/journals/jamaneurology/fullarticle/2764548; Department of Neurology and Weill Institute for Neuroscience, University of California, San Francisco.
Endothelial cell infection and endotheliitis in COVID-19; Zsuzsanna Varga; Andreas J Flammer; Peter Steiger; Martina Haberecker; Rea Andermatt; Annelies S. Zinkernagel et al. Published: April 20, 2020; DOI: 10.1016/S0140-6736(20)30937-5 https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(20)30937-5.pdf
Facing COVID-19 in the ICU: vascular dysfunction, thrombosis, and dysregulated inflammation; Safiya Richardson, MD, MPH1,2; Jamie S. Hirsch, MD, MA, MSB1,2,3; Mangala Narasimhan, Published online April 28, 2020. https://link.springer.com/article/10.1007%2Fs00134-020-06059-6
Incidence of thrombotic complications in critically ill ICU patients with COVID-19; F.A. Kloka, M.J.H.A. Kruipb, N.J.M. van der Meerc, M.S. Arbousd, D.A.M.P.J. Gommerse K.M. Kantf, F.H.J. Kapteina, J. van Paassend, M.A.M. Stalsa, M.V. Huismana,1, H. Endeman, DOI: 10.1016/j.thromres.2020.04.013 © 2020 Published by Elsevier Ltd https://www.thrombosisresearch.com/article/S0049-3848(20)30120-1/pdf
Acute ischemic stroke with COVID-19: an international consensus statement; Qureshi AI & al. Int J Stroke 03.05.2020 https://www.univadis.de/viewarticle/acute-ischemic-stroke-with-covid-19-an-international-consensus-statement-719799
COVID-19-Related Stroke; David C. Hess; Wael Eldahshan; Elizabeth Rutkowski; Translational Stroke Research; DOI: 10.1007/s12975-020-00818-9; 06.05.2020 https://link.springer.com/article/10.1007/s12975-020-00818-9
Blood Clots & Strokes in COVID-19; ACE-2 Receptor; Oxidative Stress
Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area; Safiya Richardson, MD, MPH; Jamie S. Hirsch, MD, MA, MSB; Mangala Narasimhan, DO; JAMA. Published online April 22, 2020. DOI:10.1001/jama.2020.6775; https://jamanetwork.com/journals/jama/fullarticle/2765184
Severe COVID-19 infection associated with endothelial activation; Robert Eschera, Neal Breakeya, Bernhard Lämmle; Letter to the Editors-in-Chief|
Volume 190, P62, June 01, 2020
Angiotensin converting enzyme-2 confers endothelial protection and attenuates atherosclerosis; Lovren F, Pan Y, Quan A, Teoh H, Wang G, Shukla PC, Levitt KS, Oudit GY, Al-Omran M, Stewart DJ, Slutsky AS, Peterson MD, Backx PH, Penninger JM, Verma S., Am J Physiol Heart Circ Physiol. 2008 Oct;295(4):H1377-84. DOI: 10.1152/ajpheart.00331.2008. Epub 2008 Jul 25.
COVID-19 and Oxidative Stress (Prevention & Risk Factors)
Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic; Eakachai Prompetchara, Chutitorn Ketloy, Tanapat Palaga; Asian Pac J Allergy Immunol 2020;38:1-9 DOI: 10.12932/AP-200220-0772; https://journals.physiology.org/doi/full/10.1152/ajpheart.00331.2008
Angiotensin converting enzyme-2 confers endothelial protection and attenuates atherosclerosis; Lovren F, Pan Y, Quan A, Teoh H, Wang G, Shukla PC, Levitt KS, Oudit GY, Al-Omran M, Stewart DJ, Slutsky AS, Peterson MD, Backx PH, Penninger JM, Verma S., Am J Physiol Heart Circ Physiol. 2008 Oct;295(4):H1377-84. DOI: 10.1152/ajpheart.00331.2008. Epub 2008 Jul 25. https://journals.physiology.org/doi/full/10.1152/ajpheart.00331.2008
ACE2 and Ang-(1–7) protect endothelial cell function and prevent early atherosclerosis by inhibiting inflammatory response;
Zhang YH, Zhang YH, Dong XF, Hao QQ, Zhou XM, Yu QT, Li SY, Chen X, Tengbeh AF, Dong B, Zhang Y.; Inflamm Res. 2015 Apr;64(3-4):253-60. DOI: 10.1007/s00011-015-0805-1 Epub 2015 Feb 27; Department of Cardiology, Shandong Provincial Hospital Affiliated to Shandong University, Jinan, Shandong, China.
Local angiotensin-(1-7) administration improves microvascular endothelial function in women who have had preeclampsia. Stanhewicz AE, Alexander LM; Am J Physiol Regul Integr Comp Physiol. 2020 Jan 1;318(1):R148-R155. DOI: 10.1152/ajpregu.00221.2019. Epub 2019 Oct 2 Noll Laboratory, Department of Kinesiology, The Pennsylvania State University, University Park, Pennsylvania. https://pennstate.pure.elsevier.com/en/publications/local-angiotensin-17-administration-improves-microvascular-endoth
Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area; Safiya Richardson, MD, MPH; Jamie S. Hirsch, MD, MA, MSB; Mangala Narasimhan, DO; JAMA. Published online April 22, 2020. DOI:10.1001/jama.2020.6775; https://jamanetwork.com/journals/jama/fullarticle/2765184
Nutrients and Oxidative Stress: Friend or Foe? Bee Ling Tan,Mohd Esa Norhaizan and Winnie-Pui-Pui LiewOxidative Medicine and Cellular LongevityVolume 2018, Article ID 9719584, 24 pages; DOI: 10.1155/2018/9719584; https://www.researchgate.net/publication/322852493_Nutrients_and_Oxidative_Stress_Friend_or_Foe
Oxidative stress in endothelial cell dysfunction and thrombosis; Joseph Loscalzo, M.D., Ph.D.; Pathophysiol Haemost Thromb 2002;32:359–360; DOI: 10.1159/000073600;
Angiotensin converting enzyme-2 confers endothelial protection and attenuates atherosclerosis; Lovren F1, Pan Y, Quan A, Teoh H, Wang G, Shukla PC, Levitt KS, Oudit GY, Al-Omran M, Stewart DJ, Slutsky AS, Peterson MD, Backx PH, Penninger JM, Verma S., Am J Physiol Heart Circ Physiol. 2008 Oct;295(4): H1377-84. DOI: 10.1152/ajpheart.00331.2008. Epub 2008 Jul 25.; https://journals.physiology.org/doi/full/10.1152/ajpheart.00331.2008
Sources
Prof. F. Ruschitzka, Director of Cardiology at University Hospital Zurich
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30937-5/fulltext
Prof. Dr. Goetz Thomalla, Hamburg, Speaker of the German Society of Neurology, Cerebrovasular Diseases
Prof. Peter Berlit, Secretary General of the German Society of Neurology (DGN))
https://www.mta-dialog.de/artikel/ist-sars-cov-2-ein-schlaganfallausloeser.html
Prof. Klaus Pueschel, Director at the Institute of Forensic Medicine, University Hospital Hamburg-Eppendorf (UKE)
https://www.acpjournals.org/aim/fullarticle/2765934/autopsy-findings-venous-thromboembolism-patients-covid-19-prospective-cohort-study
Wichmann D et al. Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study. Ann Intern Med. 06.05.2020
Roger D. Seheult, MD, Pulmonologist, Banning Specialty Care Center, California, USA
Coronavirus Pandemic Update 61: Blood Clots & Strokes in COVID-19; ACE-2 Receptor; Oxidative Stress https://www.youtube.com/watch?v=22Bn8jsGI54
Coronavirus Pandemic Update 65: COVID-19 and Oxidative Stress (Prevention & Risk Factors) https://www.youtube.com/watch?v=gzx8LH4Fjic
Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China Ling Mao; Huijuan Jin; Mengdie Wang; et al Yu Hu; Shengcai Chen; Quanwei He; Jiang Chang; Candong Hong; Yifan Zhou; David Wang; Xiaoping Miao; Yanan Li, MD, PhD; Bo Hu, MD, PhD JAMA Neurol. published online April 10, 2020. doi:10.1001/jamaneurol.2020.1127 JAMA Neurol. published online April 10, 2020. doi:10.1001/jamaneurol.2020.1127
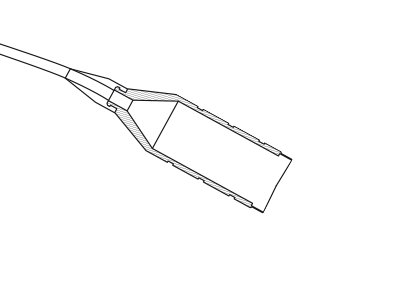
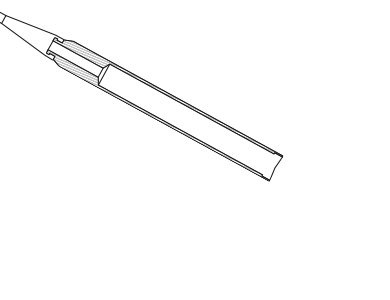
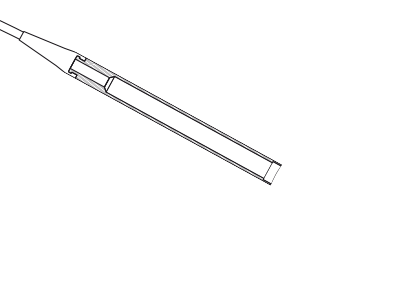
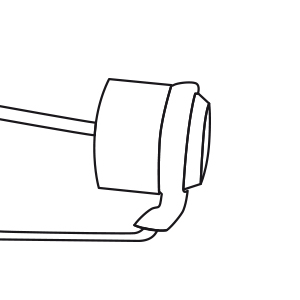
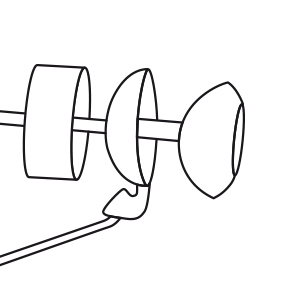
Illustrations exemplary. Findings depending on sex and age.